3 Year Celebration, another year has come and gone
Wow, it’s hard to believe three years have passed since my heart attack. That’s three years of laughs, hugs, new friendships and celebrating life! Never in my wildest dreams did I think that I would still be telling my story. Hey, my names Melissa and I had a heart attack!! But talking with people and sharing my crazy heart attack ride has opened my eyes to the need to help others. The thing about having a heart attack is there’s no outward sign telling people about your journey. Many times we recover in private and act like it didn’t happen. We may be too embarrassed and think that we did something to cause it. I didn’t exercise enough! Was my diet crappy? Maybe, I’m too stressed out? We are often too quick to move on and get back to the hustle and bustle of life. This needs to stop, and we need to TALK!!!
Just within the past two weeks, I have met two women both in their 40’s who’ve had a heart attack. It's funny how we all look at each other like you have to be kidding... Right? Had I not so publicly shared my story and went on as nothing happened I would have never had the opportunity to help others. Many times I’ll ask Joe do you think people are getting sick of me yet?? And of course, being the amazing husband, he always says no. I have to thank Joe for being the one to inspire me to continue writing this blog. This has led me to meet so many amazing people at the American Heart Association who also have the same purpose, to end the #1 killer!
I celebrated my three-year heartiversary this past weekend. To be honest, it dredged up some not so fun memories of the night I had my heart attack. You start to remember the feelings of, is this happening? I am way too young? Why me? Nuts, could this happen again, what if the stents have started to block? But then you look around and see your beautiful family and remember that you are here for a reason so don’t let it go to waste.
With February being heart month I’m trying to increase education around heart attack symptoms, hands-only CPR and furthering the cause of the American Heart Association. So like it or not your gonna be hearing a lot from me!
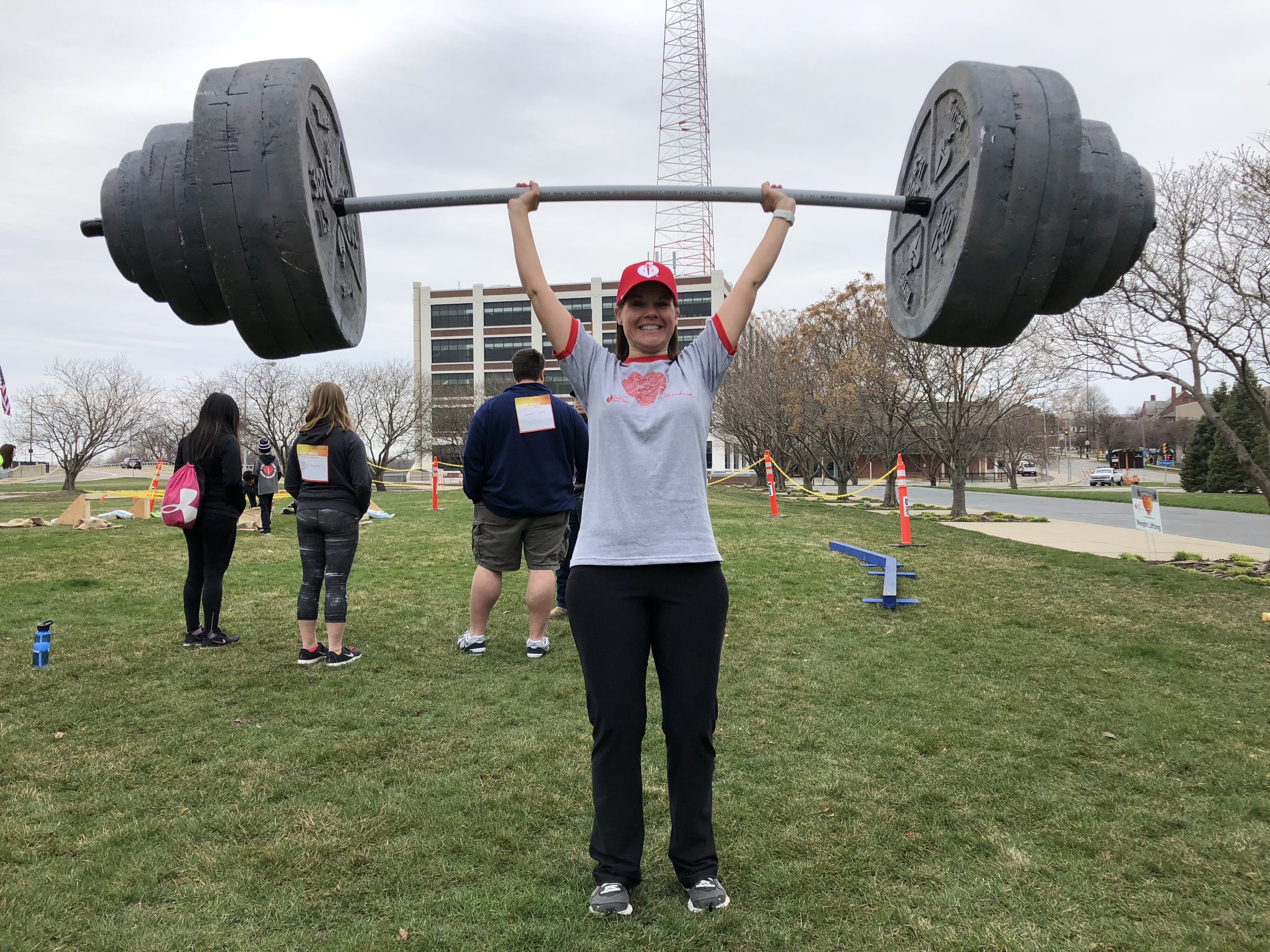
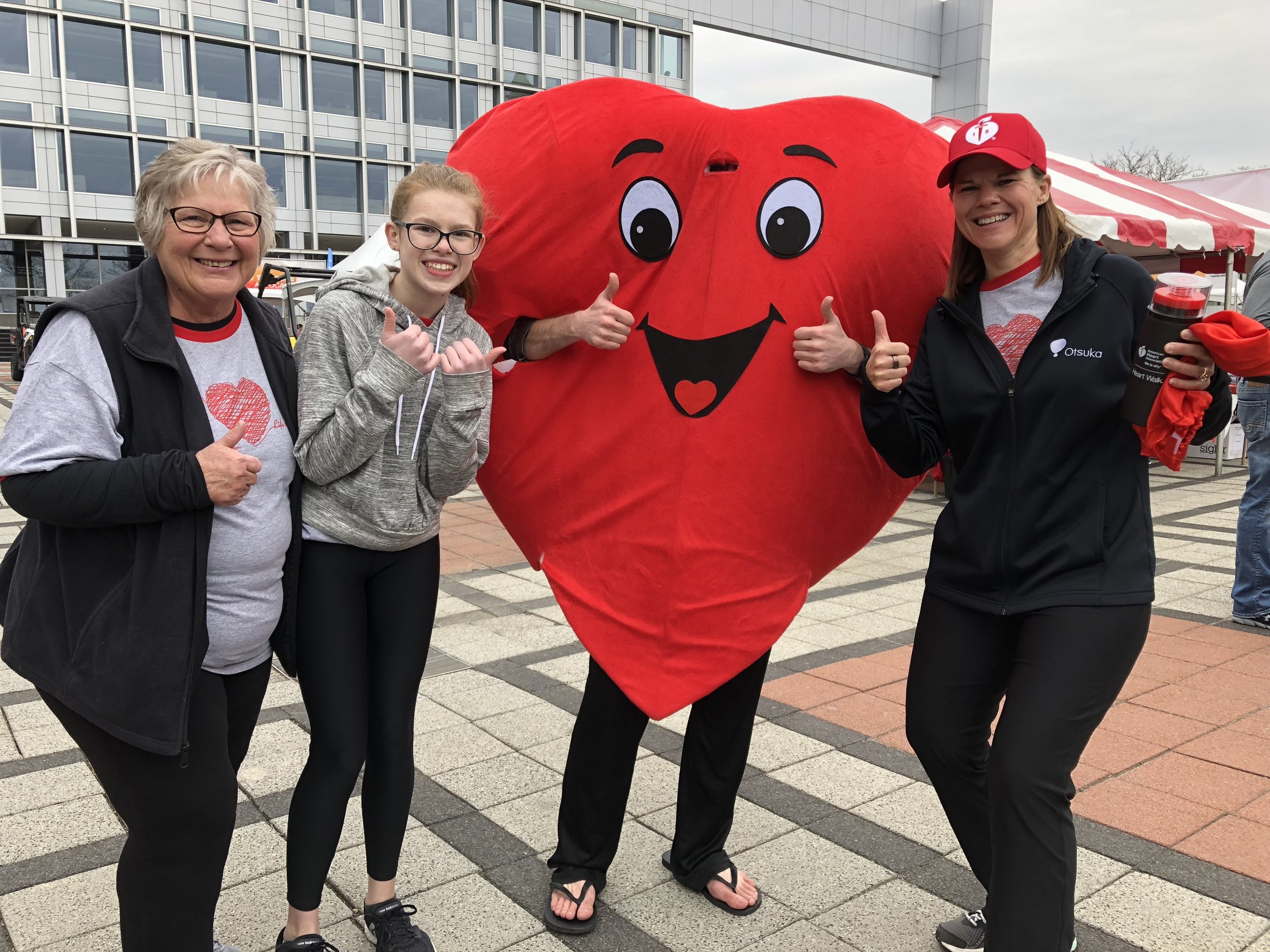
Below, are a few of the fun photos from the events that I have been able to attend and get the word out about not being a heart attack victim but a HEART WARRIOR!
DSM Heart Ball 2019
Ken, Colleen and Kurt’s Valentine’s Day Radiothon
Wear Red Day 2-1-19
In closing, thank you for taking the time to read my blog and facebook posts. I hope you never have to share your story with me! So let’s work together to get the word out about heart disease and put an end to a devastating problem!!